For many individuals living with depression, standard treatments such as medication and talk therapy provide meaningful relief. Yet for others, symptoms persist despite multiple attempts at recovery—a condition known as treatment-resistant depression. This challenge has spurred researchers and clinicians to explore new pathways, blending neuroscience, technology, and holistic care. From rapid-acting medications and non-invasive brain stimulation to digital tools and integrative wellness practices, today’s approaches are redefining what’s possible in managing stubborn forms of depression. These innovations offer renewed hope and emphasize a more personalized, patient-centered vision for mental health care.
What Is Treatment-Resistant Depression?
Major depressive disorder (MDD) is a prevalent mental health condition affecting people from all walks of life. For a significant portion—about one in three individuals—traditional antidepressants and psychotherapy alone do not lead to meaningful improvement. This scenario is described as treatment-resistant depression (TRD), which often requires alternative strategies and tailored care. Access to the latest treatment information about emerging and established interventions is vital for patients seeking relief from persistent symptoms.
The journey with TRD can feel frustrating, but ongoing advances in the field offer renewed hope. As clinicians deepen their understanding of the brain and its complex interactions, pathways have opened for individuals who previously felt out of options. Exploration of new therapies and technology-based treatments is expanding patients’ choices, making it essential to stay informed about what may be available beyond traditional medication and talk therapy.
Modern Treatment Approaches for Resistant Depression
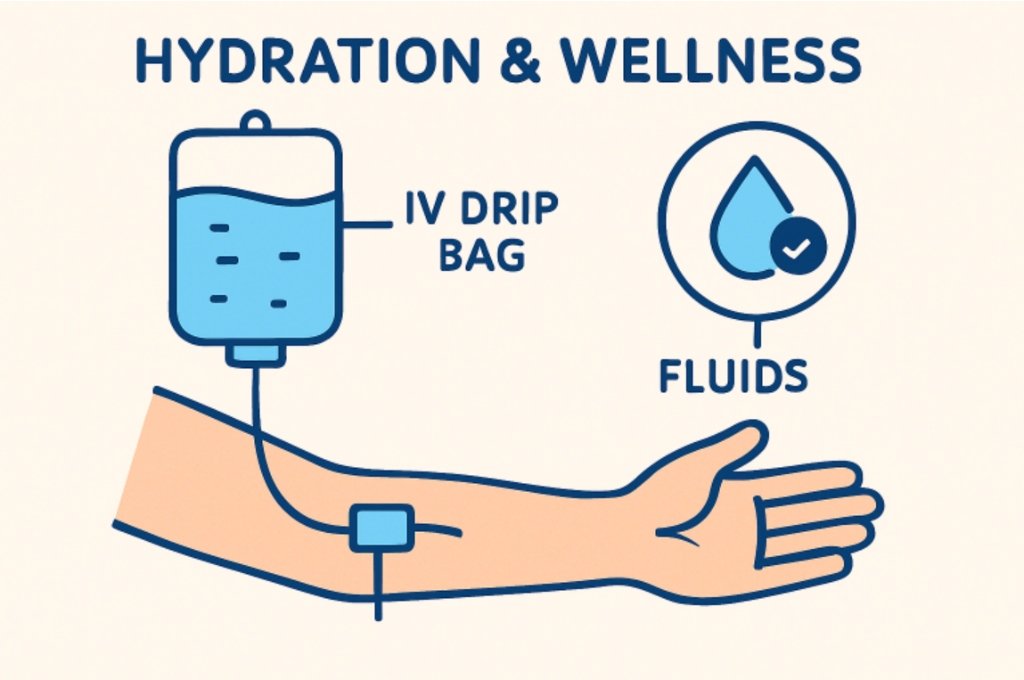
Standard antidepressants and cognitive behavioral therapy are the usual first-line approaches to treating depression. However, clinicians expand the toolkit when these efforts do not yield meaningful improvement after several attempts and adequate doses. Approaches for TRD include combining several medications, changing drug classes, or adding medications that target biological pathways differently. For some, intensive options like esketamine nasal spray and intravenous ketamine have become life-changing interventions, supported by strong clinical evidence and FDA approval in some instances.
Importantly, newer technologies and therapies now sit alongside medication adjustments. Transcranial magnetic stimulation (TMS) and neurofeedback, for example, have developed into valuable adjuncts for those with stubborn symptoms.
The Role of Neuromodulation and Brain Stimulation
Neuromodulation refers to treatments that directly or indirectly alter brain activity as a therapeutic intervention. Two of the most recognized forms are TMS and electroconvulsive therapy (ECT). Both are recommended for cases where medications and talk therapy have proven insufficient. TMS, in particular, uses magnetic fields to activate targeted brain areas involved in mood regulation, offering a noninvasive, relatively well-tolerated option. ECT, while older, remains one of the fastest-acting treatments for severe and refractory depression, especially when suicidality or catatonia are risk factors.
Recent research highlights promising advances in these methods, including more precise targeting, reduced treatment duration, and refined protocols that improve comfort and minimize cognitive side effects. These improvements help ensure that even those once considered untreatable have a path forward.
Accelerated Depression Treatments: A Fresh Look
Innovations in treatment delivery are dramatically reducing the time it takes to see an effect. Accelerated brain stimulation protocols, such as delivering multiple TMS sessions per day over a condensed schedule, have captured the attention of both clinicians and patients seeking rapid improvement. This strategy is desirable to those struggling with severe symptoms or life disruptions, as early studies indicate significant symptom reduction in just days or weeks, a departure from the months-long process often seen with conventional therapy.
While these approaches are not the norm everywhere, authoritative research from reputable institutions like the National Institute of Mental Health underscores these therapies’ growing evidence base and promise. Working with experienced clinical providers remains crucial to ensure accelerated protocols are a safe and suitable fit.
Deep Dive: Case Examples From Recent Studies
Recent trials are refining our understanding of TRD and who benefits most from new therapies. An NIH study found that patients who failed multiple interventions improved after accelerated brain stimulation, with some regaining full function and others showing increased resilience and hope. Detailed patient profiles and adaptable interventions foster a personalized, dynamic approach to care. Patients and providers should stay open to changing strategies if initial efforts fail. Ongoing monitoring and real-world feedback guide best practices and future mental health innovations.
Working with a Clinical Team: Steps to Take
To improve recovery from a condition, provide a detailed history of past treatments and their effects, as this helps clinicians create personalized care plans. Consider the latest interventions, such as device-based therapies or accelerated scheduling, if conventional methods haven’t worked. To address potential complications, request a comprehensive evaluation, including physical and mental health screenings. Consider advanced options like pharmacogenetic testing or neuroimaging for personalized treatment. Maintain consistent communication with your care team to address any new side effects or relapses.
Finding Support and Resources
The journey with treatment-resistant depression is long and lonely, but connecting with support groups, professionals, or credible sources like the National Institute of Mental Health reduces isolation. Recovery is rarely straightforward, but with advanced treatments, ongoing research, and collaboration, progress is more achievable than ever.
Conclusion
Treatment-resistant depression may feel overwhelming, but it is no longer synonymous with hopelessness. Advances in science, technology, and clinical practice have broadened the landscape of care, offering multiple pathways for recovery where once there were few. From brain stimulation therapies to accelerated protocols and tailored medication strategies, patients today have more options than ever before. Equally important is the role of supportive networks—family, peers, and trusted healthcare providers—who help ensure that no one has to navigate TRD alone. With persistence, openness to innovative approaches, and collaboration with skilled clinicians, many individuals can find relief and regain a sense of stability, purpose, and hope for the future.